A T-score compares an adult’s results with the mean peak bone mass (thickness of bones) of a large number of normal females and males between the ages of 20-40.
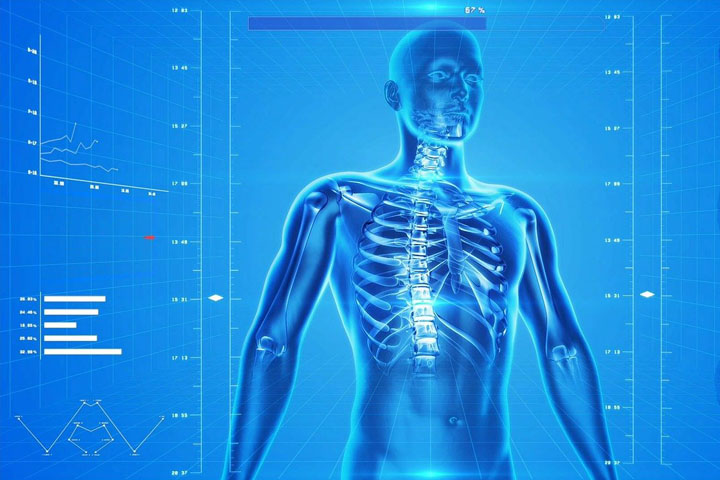
A DXA scan is like having an X-ray. It is completely painless, and it is not claustrophobic. You lie on your back for approximately 10-15 minutes while a bar moves back and forth above you.
A DXA scan measures a person’s bone mineral density, which tells the condition of the person’s bone health.
It is essential that all cause/s of your bone loss are investigated and addressed, in order that your bone health can be improved. Certain blood tests are also recommended to assist in finding the causes of your bone loss. Example low levels of Vitamin D are very common in Ireland, so your level needs to be checked, which is done by a blood test.
The DXA scan measures the bone density in your lower spine: The 1st, 2nd, 3rd, and 4th Lumber vertebrae, which are the bones in your lower back, below your belt line and it measures one or both hips. The IOS (Irish Osteoporosis Society) recommends that both hips are scanned unless you have had a hip replacement.
A DXA with an LVA (Lateral Vertebral Assessment) is a Lateral view (side view) DXA scan of the low, mid, and upper back, to rule out fractures (Broken bones) in these areas. When having a DXA with an LVA, you will be asked to turn and lie on your side.
An LVA needs to be requested on a referral letter. If an LVA is not available, a lateral thoracic X-ray should be done, to rule out fractures in the bones in the mid and upper back, which a regular DXA scan does not scan this area.
DXA scan results are sent back to your GP or the referring consultant.
We recommend re-scanning at a minimum of every two years (preferably on the same machine). It is essential that your response to treatment is monitored.
When you are re-scanned, your new results should be compared to your last DXA scan results, to ensure that you have improved. Your results should not decline, if this happens, why you have declined should be investigated.
A T-score compares an adult’s results with the mean peak bone mass (thickness of bones) of a large number of normal females and males between the ages of 20-40.
A Z score compares the patient’s score with their own age group: this is usually used in the diagnosis of the spine in children and adolescents. Their bone age should also be compared to their chronological age by taking an x-ray of the bones of their non-dominant hand.
The IOS has broken up the scores in the osteopenia range to make it easier for people to know exactly where they are on the scale.
A fragility fracture (broken bone from a trip and fall from a standing position or less) is also considered to be Osteoporosis unless proven otherwise.
Research shows that most fractures (broken bones) occur within a T score of -1.5 to -2.49 which is the moderate to marked Osteopenia range
If a person has developed a hump on the back, an LVA (Lateral Vertebral Assessment) of the thoracic spine (the area where the hump is located) is usually recommended if available. If not available, a lateral x-ray of the spine is advised. This will show if the shape of the bones in this area are compressed due to an Osteoporosis fracture.
NOTE: Many people have arthritis and Osteophytes (extra bony spurs) which may have developed on the lumbar spine, which can give a false higher bone density reading. This would make your bones appear healthier than they are.
A DXA scan usually only measures your lumbar spine (lower back = L1, L2, L3 and L4) and your hips, neck of femur and greater trochanter. The upper back (LVA) is usually not done unless specifically requested on the referral form.