These non-hormonal medications work by reducing the rate a person is losing bone which decrease the person’s risk of breaking bones. Brand names include Boniva®, Fosamax® and Fosavance®.

Osteoporosis is a condition that affects the inside of bones. It causes bones to become fragile, so they break easily. It is called the silent disease because there are no signs or symptoms prior to a person breaking (fracturing) bones. The effects of undiagnosed/untreated osteoporosis can be devastating, therefore the prevention and early detection of this disease is so important.
Bone is a living tissue that the body continually removes and replaces. As we get older, this process slows down, and usually more bone is lost than formed. However, some people lose bone much faster than others, when new bone formation does not keep up with the loss of old bone, it will result in osteoporosis.
It is estimated that up to 300,000 people in Ireland have osteoporosis. Although more common in females who have gone through the menopause, it can also affect men and even children.
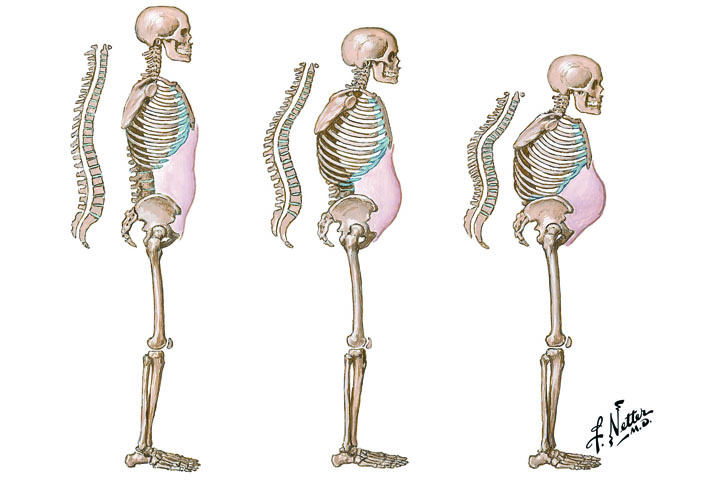
Osteoporosis can occur in any bone in the body, however some bones are more at risk to breaks than others. The most common bones to fracture are the bones in your wrist, your hip bones, and the bones in your back. With osteoporosis, a trip and fall can result in broken bone’s. A break can also happen while carrying out everyday tasks such as bending down, standing up from a chair, even when coughing. This is why anyone who has unexplained broken bones should be assumed to have Osteoporosis, unless they are investigated, and Osteoporosis is ruled out.
Broken bones due to bone loss are also known as low trauma fractures, osteoporotic fractures, and fragility fractures, and can have devastating consequences, especially in senior citizens. When you break a bone, you can have trouble with dressing, bathing, and even walking, which can lead to a person losing their independence. Unless your causes of bone loss are investigated and addressed, you can continue to lose bone and can end up with more broken bones.
You can reduce your risk of experiencing a break, as most are preventable. Osteoporosis is treatable, and there are plenty of steps you can take to maintain healthy bones. Medications are available to treat bone loss and they can help to significantly reduce your risk of fractures, combined with healthy eating and appropriate exercise.
Osteopenia is the early stage of bone loss and is diagnosed by having a DXA scan of your spine and hips. It is very important that your causes of bone loss are investigated and addressed, to help reduce your risk of developing Osteoporosis. Research shows that most broken bones occur in the moderate to marked Osteopenia range.
Osteoporosis and Osteopenia risk factors outside your control include the following:

Physical activity: If you spend most of your day sitting, then you have a higher risk of developing osteoporosis than those who are physically active.
Smoking: Not only is smoking bad for your general health, but it is also known to negatively affect bone health.
Excess alcohol: Regularly consuming more than two alcoholic drinks a day increases your chances of developing osteoporosis.
Diet: Calcium and vitamin D are essential for bone health. If you are not getting the daily recommended amounts, then you may be at increased risk of breaking bones.
Excess caffeine affects bone health.
Excess Fibre: we recommend not to take more than 30 grams of fibre a day.
Eating disorder / over-exercising or both: Please reach out for help as the secondary effects of these can cause significant bone loss, as well as affecting your overall health and fertility. Loss of periods is common with these issues.
Vegan we recommend people eat a variety of foods, not limit themselves to certain foods, especially when it can place a person at risk of bone loss. All vegans should get a DXA scan done and monitor their bone health throughout their life.
Women are at the highest risk of developing osteoporosis. However, men and children can also be affected. Furthermore, athletes who overtrain, those who develop eating disorders, or a combination of both can be at high risk to develop Osteoporosis when they are young and without help can end up not being able to compete due to the secondary effects of untreated Osteoporosis.
While no one experiences signs or symptoms before breaking a bone, there are signs and symptoms of possible undiagnosed osteoporosis.

If you are at risk of bone loss, a DXA scan, which is similar to an X-ray, is the only test the Irish Osteoporosis Society, who are the national leading experts in Ireland recommend. A DXA scan measures your bone density, which is the quality of your bone and the results will show if you are at risk of breaking bones.
A DXA scan: is not claustrophobic; it is painless and takes about 20 minutes to complete. A scan is taken of your spine and hips and your DXA scan results are in numbers called T-scores. Your doctor will be sent a copy of your DXA scan results, and it is essential to discuss what the results mean for you, as most broken bones are preventable.
We recommend DXA re-scanning a minimum of every two years, once a year if possible, so that your response to your osteoporosis treatment is monitored. This is very important in case your results are declining instead of improving.
Osteopenia: Your doctor may tell you that you have osteopenia, which is the early stages of osteoporosis. The causes of your bone loss must be investigated and addressed, to prevent you from losing more bone and developing osteoporosis. If your DXA scan says you have Osteopenia but you have broken a bone, we would consider you to have Osteoporosis, and a treatment plan needs to be initiated, as research shows that the majority of broken bones occur in the Osteopenia range.
If you take our risk factor test on this website and the results say you are at risk of bone loss, please make an appointment with your GP to further discuss your bone health plan. Your doctor should advise you on what you need to do. We have developed a checklist of questions to ask your doctor to help you improve your bone health.
Many people believe that a DXA scan contains a significant amount of radiation, but this is not true. A DXA scan contains 10% radiation of a regular Chest X-ray and anyone who has flown to New York from Dublin would have been exposed to more radiation on the flight, then having a DXA scan done.
The Irish Osteoporosis Society only recommend taking medications and treatments that have had extensive clinical research done on them, to prove they actually work. Osteoporosis treatments either help to prevent bone loss or increase bone formation, which reduces your risk of breaking bones.
The best choice for you depends on your DXA scan results, the causes of your bone loss, your risk of breaking bones, your age, gender, and medical history.
Possible treatments include the following:
These non-hormonal medications work by reducing the rate a person is losing bone which decrease the person’s risk of breaking bones. Brand names include Boniva®, Fosamax® and Fosavance®.
Oestrogen and progesterone can be prescribed for females with low oestrogen either as HRT for postmenopausal women, if they do not have contraindications or the contraceptive pill for premenopausal women. HRT prevents bone loss.
Also used as a breast cancer treatment, these drugs work similarly to oestrogen. They are often prescribed for women who experience side effects from HRT. The most well-known brand is Evista®.
This drug (brand name Prolia®) works by reducing bone loss, so more bone is maintained then lost and it is a twice-yearly injection.
Forsteo is the most well-known brand name. This is a daily injection for severe osteoporosis. PTH is a bone-forming agent that stimulates new bone growth.
One of the main causes of bone loss in men is low testosterone levels, which is why it is essential testosterone levels are checked, as testosterone therapy may be necessary in some males.
This is a non-surgical procedure involving inserting a needle containing a special ‘bone cement’ into a broken vertebra. This procedure is not suitable for everyone and should only be done for pain relief, not to restore height.
During surgery, a balloon filled with ‘bone cement’ is placed within the broken vertebra. This procedure is not suitable for everyone and should only be done for pain relief, not to restore height.
Like all medications, there are possible risks of side effects, however, for people with osteoporosis, the high risk of breaking bones and losing your independence, usually far outweighs the risk of any possible side effect.
The good news is that diet, and appropriate exercise can help strengthen your bones, combined with an Osteoporosis prescribed medication. We do not recommend that people attempt to treat bone loss with just diet and exercise and supplements, as Osteoporosis is a disease.
Osteoporosis diet: Calcium and vitamin D are essential for healthy bones. Eating foods with calcium and vitamin D can make a difference, not only for your bone health but your overall health.
Foods that have great amounts of calcium in them include all dairy products – milk, cheese, and yoghurt. If you are vegan (you are at higher risk of bone loss) or if you are in the 5% of people in Ireland who are lactose intolerant, green vegetables are an excellent source, especially kale, Collards, and okra. Fish such as tinned salmon and sardines are also excellent choices, as well as fortified breakfast cereals.
Sunlight is an excellent source of vitamin D, but it is essential to put sunblock on after 15 minutes. Those who burn easily should not try to get their vitamin D from the sun. Great sources of Vitamin D are fortified milks, fatty fishes – salmon, tuna, and mackerel plus egg yolks.
Osteoporosis and exercise: Appropriate regular weight bearing exercise is good for you overall health and mental wellbeing. Certain exercises can also help to improve your balance and coordination, which then help to reduce your risk of losing your balance, that can lead to broken bones.
If you have bone loss or want to prevent it, weight-bearing exercises are the best type to do. If possible, you should be assessed by a chartered physiotherapist, before undertaking any exercise programme. Go for a light walk, use the stairs rather than the lift or escalator. Dancing provided you have good balance, and low-impact exercises are also options. Swimming and cycling, although good for your health and fitness, are not weight-bearing exercises. Many stretches in yoga are not recommended for Osteoporosis but also for those with arthritis. Contact the Irish Osteoporosis Society for guidance in this area.
It is possible to enjoy life while managing your osteoporosis.
Alongside taking your medications, exercising regularly and eating a healthy diet, it is essential to make your home safe to prevent trips and falls. For people living with osteoporosis, falls often cause broken bones. There are several things you can do to reduce the risks in your home, for you and your loved ones.